| Junctional Tachycardia | C7, C8, R28 | |||
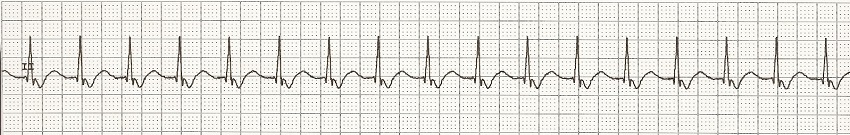
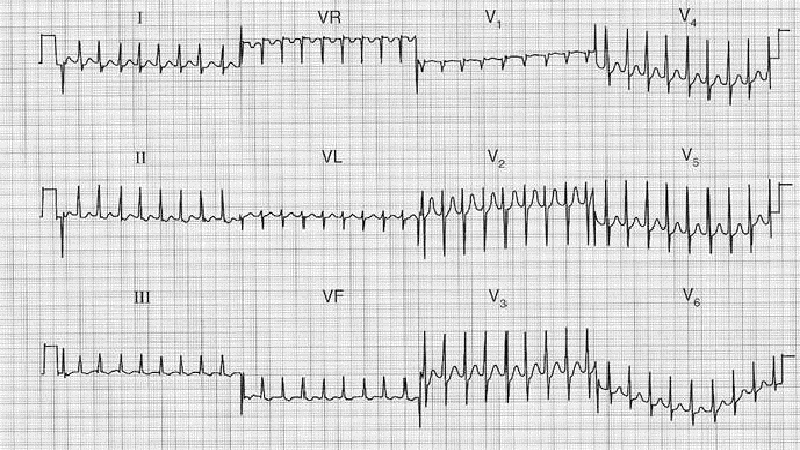
A form of supraventricular tachycardia associated with the generation of impulses from a focus in the region of the atrioventricular node due to A-V disassociation. The AV junction's intrinsic rate is 40-60 bpm. Therefore, an Accelerated Junctional rhythm is from 60-100 bpm, and becomes junctional tachycardia at a rate of >100 bpm. It can coexist with other supraventricular tachycardias due to the disassociation between the SA node and the AV node. Junctional tachycardia can appear similar to atrioventricular nodal reentrant tachycardia (AVNRT), where when a reentrant circuit forms within or just next to the AV node “The surface electrocardiographic findings of Juctional Ectopic Tachycardia (JET) can be variable, depending on whether the tachycardia is paroxysmal or incessant, and on whether ventriculo-atrial (VA) conduction occurs during tachycardia. An incessant JT with 1:1 VA conduction will present as a regular narrow-QRS tachycardia with short RP interval and retrograde P waves, mimicking typical AV nodal reentrant tachycardia (AVNRT). By contrast, in paroxysmal JET without VA conduction, the electrocardiogram (ECG) will show an irregular narrow-QRS tachycardia with intermittent sinus capture beats. During periods of frequent irregular junctional ectopy without obvious P waves or with variable distortion of sinus P waves, the surface ECG can mimic the appearance of multifocal atrial tachycardia or atrial fibrillation. Finally, JT with bundle branch block can mimic ventricular tachycardia involving the specialized conduction system, particularly if VA conduction is absent.” From: Douglas P Zipes, M.D. and Jose’ Jalife, M.D.: “Cardiac Electrophysiology From Cell to Bedside”; Sixth Edition; 2014 Elsevier Ltd. ISBN: 978-1-4557-2856-5 Junctional Tachycardia presents:
|
||||
| Rhythm Strip | ||||
 |
||||
| 12 Lead EKG | ||||
 |
||||